- Prospective Risk Adjustment
Experience our collaborative service model designed to transforming reimbursement and patient care
Enhanced Patient Care and Timely Detection
Enhanced Patient Care and Timely Detection

Offers Audit Trail of evidence so tracking clinical data and its mapping to HCC codes becomes easy.
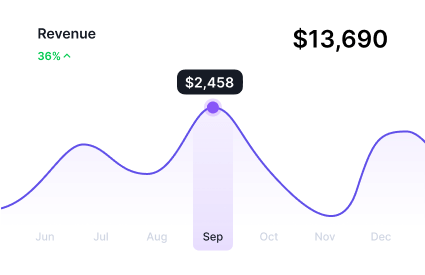
Real-time Reporting results in optimized teamwork & better utilization of time & resources.
Automated extraction & enriching of clinical data saves time & allows to focus on other core work areas.
Utilizing outsourced pre-visit planning services offers value-based care organizations multiple benefits, including cost savings, streamlined workflows, and enhanced clinical coding & documentation quality, resulting in improved patient outcomes & Compliant ROI
Our suspect analytics identify members for risk-adjustable but undocumented conditions, improving patient care.
Our prospective coding enhances accuracy in capturing patient conditions, improving risk score calculations.
Our AI solution identifies risks, suggests prevention, and refines care strategies.
Our suspect analytics identify members for risk-adjustable but undocumented conditions, improving patient care.
Our prospective coding enhances accuracy in capturing patient conditions, improving risk score calculations.
Our AI solution identifies risks, suggests prevention, and refines care strategies.
Leveraging ML/DL algorithms, our prospective risk adjustment technology enhances documentation precision and efficiency by proactively identifying suspect conditions. This automation streamlines patient chart audits, ensuring HCC and ICD-10-CM codes are accurately documented according to MEAT criteria and federal guidelines.

Our Clinical NLP algorithms can quickly analyze text and pull out vital info so you can focus on caring. Plus, fewer coding errors mean more accurate healthcare documentation.

Our Intelligent OCR platform contributes to the summarization of patient records enabling healthcare professionals to quickly review and comprehend essential details during patient consultations.

Our Smart APIs securely link clinical teams, facilitating seamless transmission of health data across various platforms. Connect with real-time results and hospitals, pharmacies, patient portals, and labs.

Our Neuro-Symbolic AI is adept at identifying inefficiencies and problems in your current coding methods, including under- and over-coding resulting in guaranteed Compliant-ROI
We consider ourselves as an integral part of your team. Our advanced technology and collaborative approach are committed to enhancing your prospective (“point of care”) risk adjustment practices, ensuring precise reimbursement, and ultimately, improving patient outcomes.

Leverage the proficiency of external coding specialists focused on extracting and validating ICD-10-CM and HCC diagnosis codes from medical records. Physicians can diminish risk and improve patient care by collaborating with adept coding review services versed in HCC Medicare regulations.
Leave all your technological concerns behind – we will take care of it. Let’s move forward from Risk to Revenue
Learn more about risk adjustment & its latest solutions for healthcare
Know more about RAAPID’s footprints online & offline
Explore RAAPID’s Collection of Case Studies for Impact We Create for Payers & Providers
