- Retrospective Chart Review
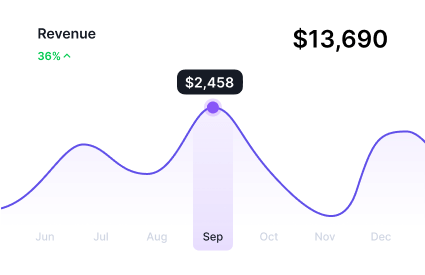
Elevate Chart Review Success with Data-Driven Insights & Expert Review
Experience unparalleled productivity and clinical accuracy with our AI-based innovative automated chart review solution with improved medical coding features, ensuring compliant ROI