- Retrospective Risk Adjustment
Maximizing reimbursements & mitigating audit risks for health plans
Increase revenue, boost accuracy, and streamline health plan workflows.
Increase revenue, boost accuracy, and streamline health plan workflows.

As per a September 2023 OIG report, acute-care hospitals received $41.4 million in improper Medicare payments due to incorrect discharge status codes.
Our AI-enabled tool aids in identifying specific unreported diagnosis codes
In a 2022 JAMA report, it's noted that ICU patients generate more than 1200 individual data points daily, with clinicians monitoring 187 alerts per patient through the EHR.
We Enable higher retrieval results through Smarter chart targeting
CMS reported collecting (Penalties) to the tune of $498 million in medicare overpayments as identified by OIG.
We ensure your Health Plan passes RADV audits, resulting in zero penalties.
OIG April 2021 report found while evaluating risk scores for 200 beneficiaries, only 1,322 (86.7%) HCCs were supported by documentation, while 203 did not. Additionally, 37 were misclassified or overlooked.
Our solution identifies potential unreported diagnosis codes and actions for further review if necessary
We process millions of medical charts automatically, resulting in comprehensive member health status & compliant ROI
Our NLP swiftly and accurately handles vast unstructured text data, with the potential to enhance patient outcomes and reduce costs. It also aids clinical decision-making, offering evidence-based diagnosis and treatment recommendations from current medical research.
Our proficient coders empower your clinical team to concentrate on primary responsibilities, delegating HCC coding reviews and audits to us. Furthermore, our healthcare experts guarantee enhanced adherence to regulatory standards, improving compliance measures for your organization.
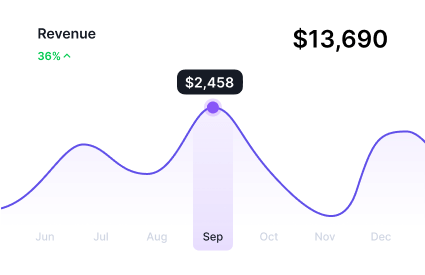
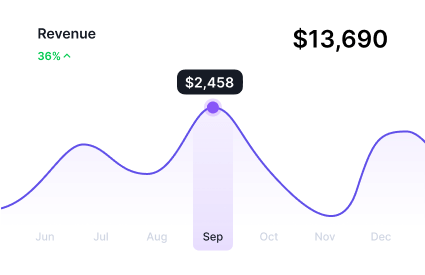
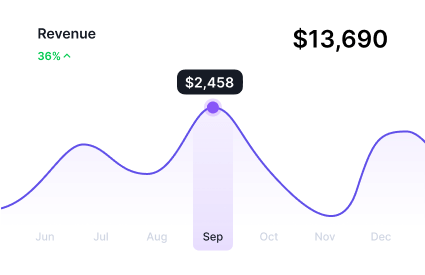
Our accurate coding practices prevent revenue loss by minimizing errors, while comprehensive HCC code reviews improve RAF accuracy. This leads to enhanced financial outcomes, ensuring better performance and compliance pertaining to financial management.
RAAPID’s AI-driven solution for retrospective risk adjustment expedites chart review processes, resulting in heightened coder productivity and precision. This technological enhancement effectively improves both output and accuracy, optimizing the overall performance of coding tasks.
For enhanced efficiency and accuracy. access our comprehensive HCC coding solution, seamlessly integrating high-risk factor diagnosis code validation and precise RAF score calculation into your current medical coding workflow
Our solutions incorporate both CMS-HCC and HHS-HCC models to provide an extensive array of customized Risk Adjustment Services, encompassing diverse data sources and formats. Our AI-powered solution leverages vast experience with a sizable repository of Medicare Advantage medical records and ACA data.
Our retrospective risk adjustment process for Affordable Care Act (ACA) plan involves a comprehensive evaluation of patient medical records that determine the health risk profile of individuals enrollees with the aim to promote fairness and equity in healthcare financing while incentivizing ACAs to provide comprehensive care to all individuals, regardless of their health status.
Medicare Advantage Organizations (MAOs) know that provider documentation frequently exceeds the accuracy of coding, understanding its profound influence on RAF (Risk Adjustment Factor) scores. To bridge coding gaps, numerous MAOs adopt retrospective chart review procedures, Our Retrospective risk adjustment solution with insightful strategies enhances the risk adjustment efficiency and performance for Medicare Advantage Organizations (MAOs)
Our NLP-powered Retrospective Risk Adjustment solutions enable payors identify and correct errors in claims, reduce the need for manual review of claims, and improve the accuracy of denials.

Our Clinical-based NLP algorithms process vast amounts of medical documentation with precision, reducing the likelihood of errors in code assignment and ensuring compliance with coding standards, resulting in Compliant ROI

Our Intelligent OCR solution automatically extracts patient data from medical records, easing indexing and enabling quick access to vital information for your risk adjustment teams

Empower your Retrospective Risk Adjustment operations with our latest healthcare APIs, enabling easy access and share medical data across EHR and other healthcare platforms, ensuring comprehensive and informed clinical decisions.

Neuro-symbolic AI algorithms mimic human intelligence to analyze retrospective clinical narratives, physician notes, and unstructured text data, extracting relevant medical codes and information with remarkable precision.
We offer a vibrant collaboration supported by our seasoned experts dedicated to ensuring confident decision-making through seamless technology integration.
Leverage our AI-driven retrospective Risk Adjustment Coding to optimize validation rates and Reduce Operational Costs.

RAAPID AI helps drive more accurate and complete coding. The auto-suggest code feature picks up code reported in the past but was not included in the current documentation.

Our RA solution features automated HCC code capture using MEAT criteria along with AI-powered diagnosis codebook, aids health plans in processing cost-effective Retrospective chart reviews.

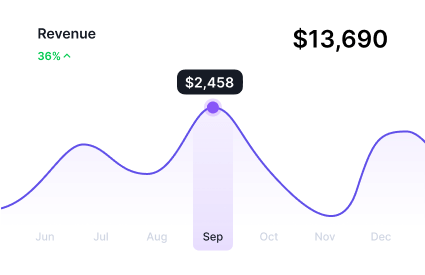
Our RA solution uses detailed analysis reports on claims processing and clinical performance trends, aiding healthcare management concerning regulatory compliance and quality improvement.

Our accurate coding practice helps process “suspect” unreported diagnosis codes to the coder, helping them focus only on those suspected conditions within the medical chart.
Leave all your technological concerns behind – we will take care of it. Let’s move forward from Risk to Revenue
Learn more about risk adjustment & its latest solutions for healthcare
Know more about RAAPID’s footprints online & offline
Explore RAAPID’s Collection of Case Studies for Impact We Create for Payers & Providers
